The following article was originally published in June of 2016, and has received a lot of interest. We are featuring it in "Editors’ Picks"
Note that this article focuses only on heart attacks, which are caused by blockages in the flow of blood to the heart, and not on sudden cardiac arrests (SCA) which involve heart stoppages caused by the heart itself malfunctioning. For more on SCA and how they differ from heart attacks, this guide (https://avive.life/guides/cardiac-arrest-vs-heart-attack/) provides an excellent overview.
The spectre of heart attacks looms large in our collective psyche. We worry that one may strike us, or perhaps one of our at-risk relatives or friends will be afflicted. Some of us at times view them as retribution for an unhealthy lifestyle. But what do we really understand about heart attacks? In this article, I (Oliver Kuhn) will cover the clinical side of heart attacks, and Steve Lynch (in italicized text) will relate his personal heart attack experience.
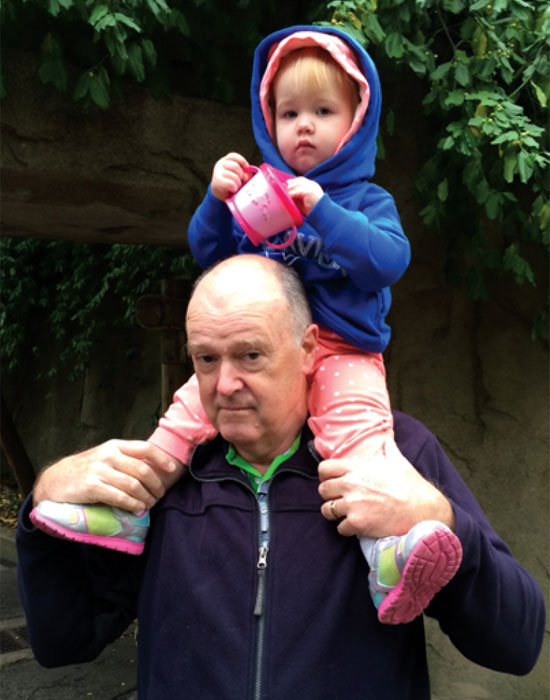
This picture was taken on October 2, 2015 at the Cincinnati zoo. I am "Horsie" on the bottom. The rider is my granddaughter Alexa; she’s trying to feed me “oats” just like her mother used to. Sadly, time has not improved the taste of soggy Cheerios. Being force-fed “oats” aside, with no concerns for my health, I carried Alexa all over the zoo and back to the car and never gave it a moment’s thought.
At the time, though, both my wife and I were thinking about other things. 2015 will go down as the year I got old and we did not know why. My blood sugar was fine, my cholesterol was fine, my electrocardiograph (EKG) was right on spec and my resting heart-rate was in the high 40’s. It’s true that my blood pressure, at times, seemed disturbingly high. But given everything else, the doctor wasn’t worried, so why should I be? He was the expert. Even so, I felt increasingly tired and dispirited, as if my life force were draining away.
Which it was, because when this picture was taken I had been alive for 22,997 days, but I had just 42 days left. Six weeks after this picture was taken, my natural life ended when I was hit by a 90% proximal left anterior descending (LAD) coronary artery lesion, a particularly nasty and often fatal form of heart attack. That I am here today is only because it is my good fortune to live in an age where dying can sometimes be just a temporary setback.
Anatomy of a Heart Attack
Figure 1 shows an actual human heart, viewed from the front, meaning all left side components are seen on the right, and vice versa, as the names are given from the heart owner’s perspective. We all know the heart is a pump that receives oxygen-depleted blood, pumps it to the lungs for oxygenation, and then receives and pumps out the oxygenated blood back to the body. But the heart is a muscle, and therefore itself needs a steady supply of oxygenated blood in order to function. Simply put, a heart attack (technically known as a myocardial infarction (MI) or acute myocardial infarction (AMI)) occurs when the supply of blood to the heart is partially or fully cut off. Muscles starved of oxygen are quickly damaged, often severely.
So what causes the blockage? Most of the time it starts with the buildup of fat inside our arteries, which tends to damage the artery walls. The “wounded” cell walls react by excreting chemicals that make the arterial walls stickier, and various substances that would normally pass through, carried by the blood flow, accumulate. These substances include inflammatory cells (neutrophils, macrophages, monocytes, eosinophils, and basophils – all released as part of the inflammatory response to an injury or presence of a foreign substance or substances), proteins, calcium, and cellular waste products, which combine with the fat to form plaque. The plaque builds up as a layer on the arterial walls, with a hard, crusty exterior and a softer interior, and this narrows the inner diameter of the arteries, restricting blood flow. Sometimes the hard shell on the plaque tears or cracks, and then blood platelets congregate and clotting of the blood occurs. It is these plaque/blood clot agglomerations that create the arterial blockages that can trigger heart attacks.
VEINS CARRY BLOOD TO THE HEART:
- Incoming oxygen-depleted blood from most of the body
- Oxygenated blood travelling from the lungs to the heart via the pulmonary vein
- Oxygen rich blood from the heart to the placenta via the umbilical vein.
ARTERIES CARRY BLOOD AWAY FROM THE HEART:
- Outgoing oxygen-rich blood to most of the body
- Oxygen-poor blood travelling from the heart to the lungs via the pulmonary artery
- Deoxygenated blood from the fetus to the placenta via the umbilical artery.
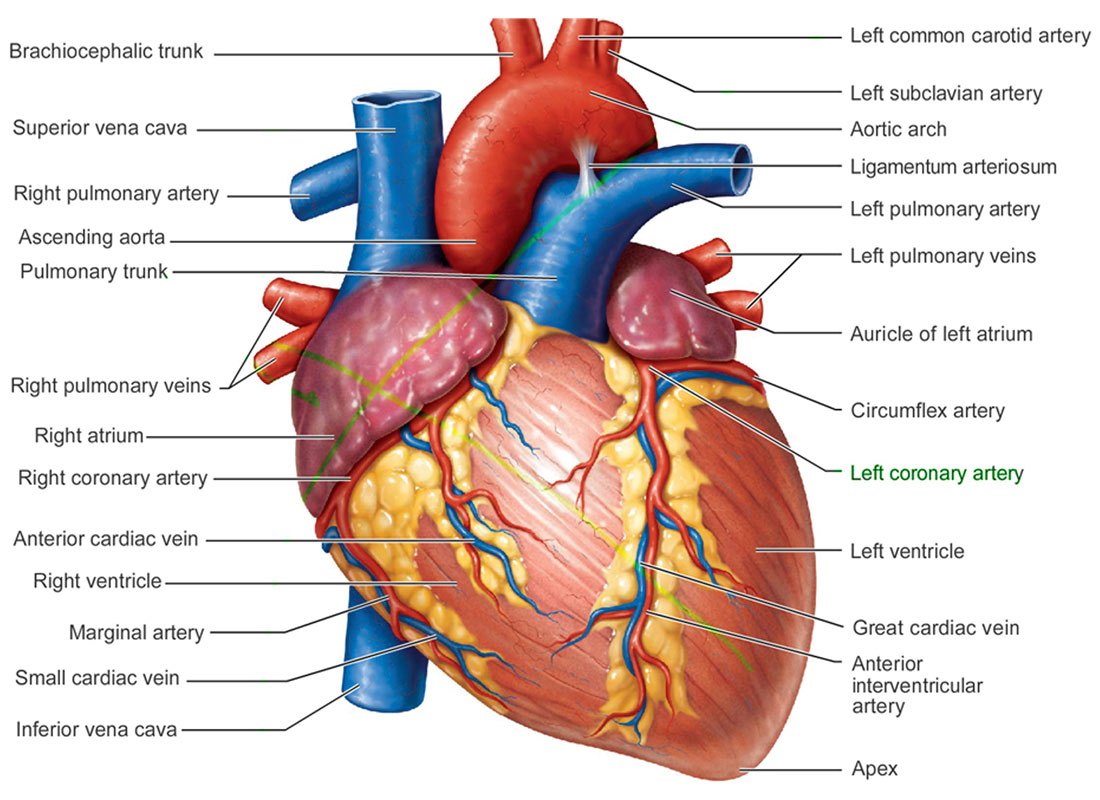
Arterial blockages can happen anywhere, but in the case of a heart attack the blockage occurs somewhere within the coronary arteries, which are inherently susceptible to blockage because they are relatively narrow. Referring to Figure 2, the right and left main coronary arteries are seen as spreading out in red across the main pump areas of the heart, the right and left ventricles. The four main coronary arteries (the left anterior descending artery and the left circumflex artery are out of view on the back side of the heart in the diagram) split into ever smaller arteries, and cover the entire surface of the ventricles, supplying the heart muscle (the myocardium) with its life blood. It is important to note that the coronary arteries represent what is known as end circulation – there is no redundancy within the system as is found elsewhere in the body, and so each coronary artery, right down to the smallest one, is the only source of blood to the part of the myocardium which it services. Because of this, blockages and the resulting heart attacks represent serious health risks to those afflicted. This statement should be qualified by saying that collateral blood vessels can develop and provide alternate routes for blood to get to the myocardium. There is evidence suggesting that strenuous exercise promotes this pulmonary collateralization.
Internally, what had happened to me was that sometime years in the past, I somehow damaged my LAD causing a slight roughness on the interior of the artery wall. Plaque started to form at the site and over decades it built up until it was by late last year blocking about 70% of the blood flow to a major region of my heart. I should at that point have been suffering from angina, chest pain caused by a lack of blood flow to the heart. That I wasn’t however, was because, thanks to my lifelong commitment to exercise, ancillary blood vessels had built up and covered the affected region.
I could have gone on that way for a long time but when we got back from Cincinnati I decided to break out of the funk that I seemed to be in by exercising myself to my limits. On Monday, October 26, I went to the gym and worked out as hard as I could, pushing my heart to its maximum. I had done this many times before and reasoned that if my heart were going to blow up it would have done it years before. In hindsight, I suspect there may have been a fatal flaw to my reasoning.
I did not break out of the funk; instead the increased arterial pressure caused a part of the plaque to break away from the arterial wall. Two things then happened within hours. First, the loose bit of plaque started to further occlude the artery. Second, a blood clot started to form at the site of the tear. Both combined to further reduce the blood flow through the artery and then the chest pains started in earnest.
Causes
The causes of heart attacks, based on statistical correlations seen in innumerable studies, are well known. Briefly, these include:
- High cholesterol
- High blood pressure
- Smoking
- Obesity
- Diabetes
- Sedentary lifestyle
- Stress
- Inherited predisposition
- Low estrogen levels (in females)
- Other factors, including bad luck (e.g. a piece of plaque or other substance finds its way to the heart and gets stuck)
In recent years there has been an emphasis within society on the factors that are controllable, and if a person has not already changed their habits and lifestyle to be healthier, then they certainly are aware of the pressure to do so and feel guilty about their inaction; many construct some internal justification, such as “I have to go sometime, might as well have fun now,” or, “No history of heart disease in my family, so I’m safe.”
Symptoms
The symptoms of a heart attack vary, but can include:
- Tightness, pain, pressure, or discomfort in chest
- Pain in neck, jaw, or shoulders
- Anxious feelings
- Shortness of breath
- Back or neck pain (especially females)
- Feeling tired, light headed or dizzy (especially females)
- Nausea (especially females)
- Cold sweat and pain moving down left arm (especially males)
- Females may experience flu-like symptoms and sleep problems ~2 weeks prior to a heart attack
The chest pains started Monday afternoon at about a level 2 on a scale of 10 (10 being a gall bladder attack). They came off and on over the week so I didn’t go back to the gym until Friday. Once I started exercising they got significantly worse so I stopped and on the Saturday I went to ER at the Foothills Hospital. There I was checked out thoroughly. They ran a series of EKG’s and blood tests to see if there was anything wrong with my heart (I didn’t think there was). The tests came back clear, however, and my EKG was exactly as it had been in 2012. I was sent home with a diagnosis of costochondritis (chest wall inflammation) and told to follow up with my family physician. Importantly though, before they sent me home, they booked me for a cardiac stress test.
By the time I saw my family doctor on the Monday the chest pains had progressed to about a level 4 in intensity. Concerned, he sent me straight back to ER and we went through the entire process again only this time far more thoroughly. I was kept in for about ten hours but again, nothing showed up on either the EKG or the blood tests. The head of cardiology actually took the time to talk with me. He assured me that he was 100% certain that it wasn’t my heart. As an aside, I don’t blame him for being wrong. It just suggests that predicting heart attacks is about as reliable as predicting earthquakes.
So I went home with a diagnosis I could support. I did not accept that my heart was causing problems. Instead, strained intercostal muscles seemed a more likely origin for the pain. I was booked for a stress test in 10 days and I was determined not to bother anyone else with my symptoms until then. I decided to just tough it out.
From this point on, things got increasingly bizarre and desperate. The pain I was feeling on the Monday was not out of the ordinary. Having played sports all my life, pain and I are old adversaries and this wasn’t anything special. That changed later in the week when I found myself trapped at the side of the road when walking my dog. What I had been experiencing up to that point was mild angina but on the Thursday it progressed to a full blown attack. I was hit by an attack of pain that literally froze me where I stood. The pain came on so quickly and with such ferocity that I simply couldn’t move and I stood where I was for about five minutes, hoping that the dog wouldn’t get anxious and pull me over. I felt that if I moved I would die. It was that simple, move and I die.
When the pain eased and I could move again I thought to sit down and call 911. But then I thought that if they carted me away in an ambulance there would be nobody to take the dog home. So I walked him home as slowly as I could and once there, with the pains subsiding I went back to my office to work. As absurd as it sounds, given that the pain had increased from level 4 to level 10, my refusal to call 911 was a typical reaction. We have no memory of pain and when it goes, as it did, we are programmed to forget about it and move on. Which I did… until the next attack.
Treatment
Once a heart attack occurs, part or all of the heart has been cut off from its blood supply, and cells start to die. This means the sooner treatment is given the better. A rule of thumb is that if a heart attack victim gets medical attention within 90 minutes of the attack their chances of surviving are much better – i.e. once the 90 minute mark is passed survival rates drop quickly.
As soon as a heart attack is suspected, it is recommended that the victim chew on some aspirin (unless they are allergic), as this thins the blood and reduces the rate of further clotting.
If the victim is unconscious, hands-only CPR doubles their chances of survival.
Once the heart attack victim is at a medical facility, the doctors will do a couple of immediate tests. First, an EKG measures the heart’s electrical activity, and can identify if a heart attack has occurred or is occurring. Areas where there is no electro-muscular activity indicate where the arterial blockage is. Second, blood tests show if proteins associated with dying myocardial cells are present.
Once the heart attack is confirmed and the location of the blockage identified, the doctor will act quickly to save as much of the affected myocardium as possible. A likely first step is the injection of drugs that dissolve blood clots.
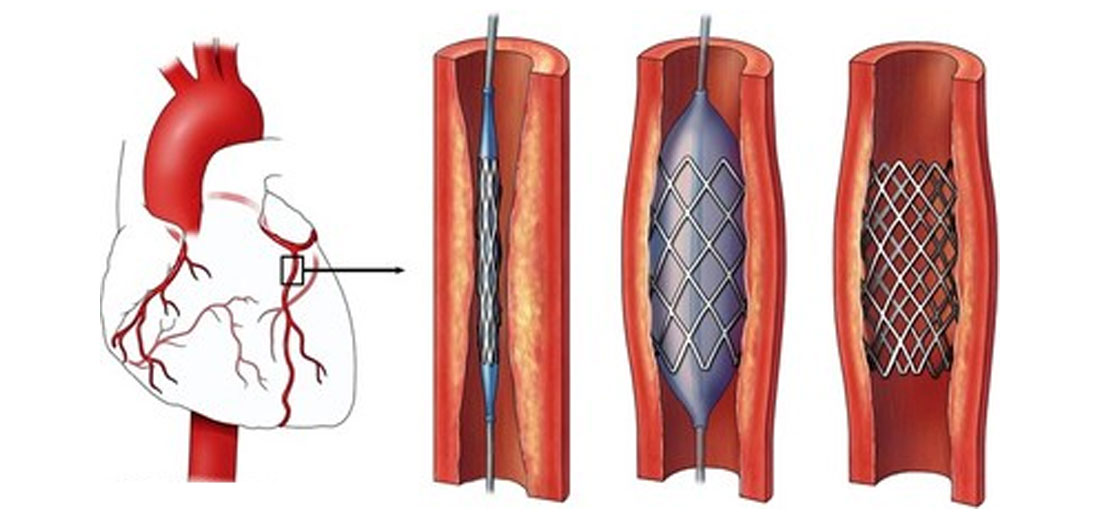
The most common surgical procedure nowadays is known as a coronary angioplasty (Figure 3). A thin tube is inserted into the relevant artery and pushed delicately through until the end is right in the middle of the blockage. At the end of the tube is an uninflated balloon surrounded by a flexible mesh known as a stent. The balloon is inflated, expanding the blocked section of artery along with the stent, which is pushed up against the artery walls. The balloon is then deflated and the tube extracted. The stent remains inside the artery, and its inherent structural rigidity holds the artery open, allowing a more normal volume of blood flow.
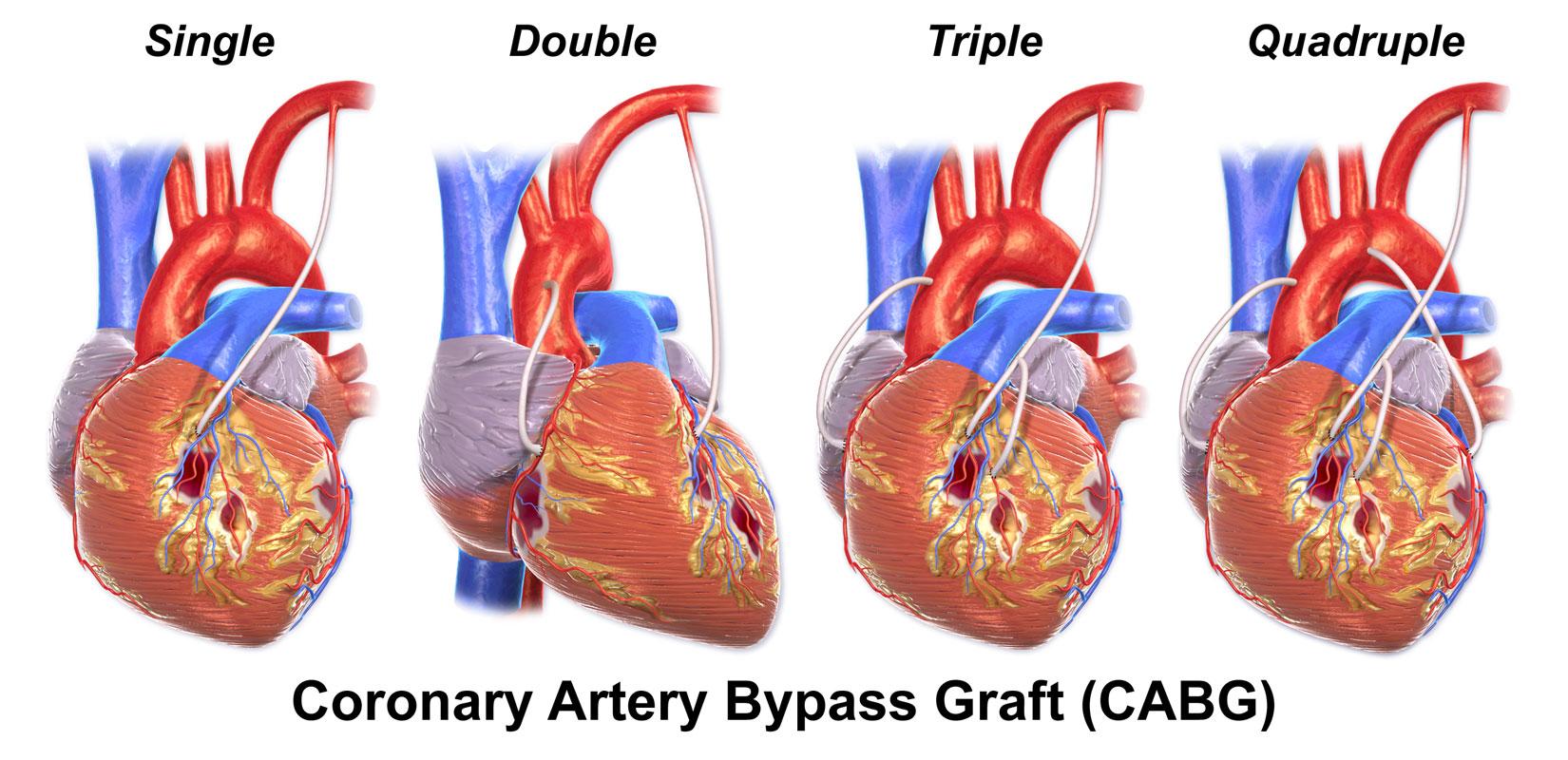
Another type of surgery is known as a coronary artery bypass graft (CABG). A section of healthy artery is taken from the patient’s leg, arm or chest, and the surgeon inserts this in such a way so as to form an alternate path for the blood to flow around the blocked artery (Figure 4).
There is no point in detailing all the attacks that I experienced over the next week. They became worse and increasingly frequent, eventually triggered simply by trying to climb one stair. The costochondritis diagnosis though, blocked all reason in my mind. I should have called 911. I should have gone back to ER. Looking back, it is absurd that I clung to the chest wall diagnosis until I went for the stress test, but I did. So do many others. The truth is that heart attacks do not occur without warning. It is just that we are programmed to ignore the warnings until we push the macho male mystique to its fatal conclusion.
When I went for the stress test on the Thursday, I was confused, frightened and desperate. My wife and I had already decided that even if this weren’t anything to do with my heart I had to go back to ER on my own. Fortunately, I didn’t have to. Up until that time I had been experiencing increasingly severe angina. But when I got up to go into the cardiologist office I had a heart attack and my heart started to die. The pain that hit me was beyond anything I believed the human body could produce. I stood there in shock and wanted to fall to the ground but I thought that if I fell, they would not be strong enough to lift me onto a stretcher. The nurse looked at me and asked if I was OK. “No,” I said, “I can’t move.”
And then all hell broke loose. We complain about the medical system but it has always amazed me how good it is when you really need it. That day, for the second time in my life, I became the most important patient in an Emergency Room. This time was different. The first time I had septicemia and was so sick that I wasn’t aware of what was happening. This time I was fully aware not just of what was happening around me but of the callous way I had dealt with the pain of the attacks and of how close my macho mentality had brought me to death. Never again I said. Perhaps this time I will mean it.
To conclude, it is now five months since the attack and in all respects I am back to normal. I got to watch them insert the stent into the artery and pop it open. Quite literally, life surged back into my body and my soul. I spent five days in the Cardiac Critical Care Unit and I have been back once to ER for what turned out to be a panic attack. Other than that, my recent echo cardiogram shows that I have, in the words of my family doctor, “a very happy heart”. Because of my ancillary blood supply, I lost very little heart muscle and what was damaged has now repaired itself.
I feel 20 years younger and there is only one small cloud in the sky. Believe it or not, I actually have costochondritis. Whether it was there before or whether it has developed as a panic reaction we don’t know. I do now know the difference and I am not worried and so I’ll end with this. Tomorrow is promised to no one. But if you work at it, you can maybe earn it.
Prevention
This of course ties back to the causes – remove or improve as many of the controllable negative factors as possible, and your chances of having a heart attack drop. Briefly:
- Stop smoking
- Exercise (~30 minutes moderate exercise / day, 5 days / week is recommended)
- Eat healthy foods, and a healthy combination of foods:
- Avoid saturated fats, such as those found in fatty meats and deep fried food
- Eat lots of fiber
- Avoid sugar
- Avoid processed foods
- Aim for a balanced diet, with everything in moderation
There is a wealth of resources on heart disease and how to avoid it. One good place to start is the Heart & Stroke Foundation of Canada: www.heartandstroke.ca.
In addition to prevention, it is good to be aware of identifying and responding to heart attacks. As we have heard from Steve, sometimes heart attacks occur due to causes that are not preventable or predictable. Knowing heart attack symptoms and how to respond is critically important.










Share This Column